By Dr. Dayanath Jayasuriya P. C.
Senior Academic Advisor (Law)- Nawaloka College of Higher Studies
(Dr. Jayasuriya was Head, UNAIDS Secretariat in Islamabad and Senior HIV/AIDS Policy Adviser to the Government of Pakistan, 2003-2004).
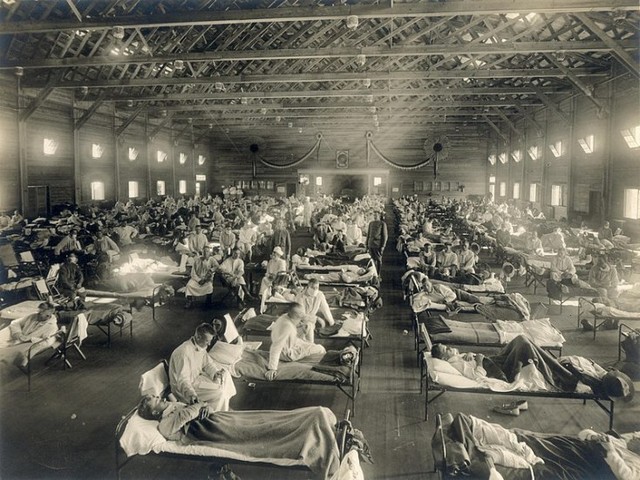
Recently there have been a few references in the media about the 1918-1919 influenza pandemic in Sri Lanka and among demographers there has been little agreement on the mortality figures. One of the leading studies was published in 1992 by C.M. Langford and P. Story of the Department of Population Studies of the London School of Economics entitled “Influenza in Sri Lanka, 1918–1919: the Impact of a New Disease in a Premodern Third World Setting” which attributed almost 50, 000 deaths.
Throughout history influenza pandemics are known to have occurred and between 1600-1900 at least nine such pandemics have been recorded. What distinguishes the 1918–1919 influenza pandemic from previous episodes is its terrible virulence. Various estimates suggest that up to 50 million would have died worldwide, including 20 million in India alone.
The Names of several countries have been suggested as to the possible geographical source of the virus- among those that have been mentioned in studies are the USA, China, Russia, West Africa, France, and Sierra Leone. Hoyle and Wickramasinghe in an article in the New Scientist attributed this and other viruses to the scattering of infective debris from comets.
According to Langford and Story “Influenza probably entered the country through the port of Colombo and possibly also through the port of Talaimannar. As elsewhere there was a mild first wave, followed by a virulent second wave characterized by fatal pneumonic complications. Women suffered heavier mortality than men and young adults more (relatively) than other age groups. Fertility fell. Probably about 1.1 per cent of the population died.”
Using Census reports and reports of Government Agents, the two authors have pointed out interesting differentials in infection and mortality rates among the two main ethnic groups: “It seems, then, that ethnic groups differed very considerably in terms of whether they suffered extremely heavy mortality from influenza in a relatively short period of time or somewhat lower mortality over a longer period, but that the longer-run differences between them, that is over six or 15 months, were very much smaller. Indian Tamils apparently suffered particularly badly in a relatively short period of time. This may well have been due to the fact that they were heavily concentrated in a residential sense in that they lived in small areas on estates and also fairly concentrated in a geographical sense in that estates were themselves concentrated in a certain part of the country. The Sinhalese, by contrast, experienced much lower peak mortality but many more months not far off that peak, so that on balance over 15 months they were not much better off than the Indian Tamils.
“This may well have reflected the fact that the Sinhalese were much more scattered both in being more likely to live in small rural communities, through which influenza may have moved more slowly, and in being distributed across many more districts in the island, where influenza arrived at different times. In the case of the Sinhalese, though, malaria would have been a factor as well as influenza; the overwhelming majority of the population in the North-Western Province, and in Anuradhapura district, were Sinhalese. It should not be overlooked, however, that even with a 15-month view of the data Indian Tamils apparently suffered more than other groups in the population. Why should Indian Tamils have experienced higher mortality from influenza than other sections of the population? Congested living conditions and low temperatures due to altitude may have played a part. However, the most important factor may well have been simply the poor state of health of Indian Tamils even in ordinary times.
“Indian Tamils were drawn from the lowest echelons of southern Indian society; and their conditions of life and work in Sri Lanka were arduous. Their mortality tended to be considerably higher than that of other groups in the Sri Lankan population. The mean expectation of life at birth for Indian Tamils computed for the combined period made up by 1900–1902, 1910–1912 and 1920–1922 was 24.0 years; the corresponding figure for the Sinhalese was 33.6 years; the figures for Moors and Ceylon Tamils were 30.3 and 31.5 years respectively. Thus, it may be that Indian Tamils suffered more than others in 1918–1919 mainly because they were already more debilitated and so at greater risk of death from influenza in the epidemic. However, it is also conceivable that the impact of influenza on this group may then have been further exacerbated by the serious food shortage that affected Sri Lanka in late 1918 and since this may well have had more effect on those, like estate workers, who depended on wages and were remote from subsistence agriculture, than on others in the population.” (references omitted).
The study contained a few other pertinent observations:
· That the epidemic seemed to strike those in the prime of life especially hard. They might have been led to this conclusion by experiencing the fact that mortality rates rose proportionally more among young adults than for any other age group.
· Women suffered heavier mortality than men during the influenza outbreak in Sri Lanka and maternal mortality rose and fertility fell. Contrary to expectation, however, the stillbirth rate did not rise but fell slightly at this time; though it is perfectly possible that the miscarriage rate may have increased during the epidemic. The heavier mortality among females was no doubt due in part to the particularly damaging impact influenza had on pregnant women; in addition the fact that female mortality was usually higher than male mortality in Sri Lanka at that time, and female health therefore presumably less good, may also have played a part.
· The influenza outbreak undoubtedly caused a great deal of disruption in Sri Lanka. Morbidity and mortality were substantial; both plantation agriculture and subsistence agriculture were adversely affected. There were many local reports of difficulty or distress because of the temporary breakdown of family and village support systems. But many communities seem to have responded to the situation fairly quickly and there was a proliferation of ‘relief committees’ organizing support for victims of the outbreak. Such activity may have been quite important in ameliorating the impact of the epidemic.
· During the last few months of 1918 and during 1919 there was quite a serious food shortage in Sri Lanka. This arose because India restricted rice exports, on which Sri Lanka was heavily dependent, and had little or nothing to do with any drop in agricultural production there might have been in Sri Lanka itself as a result of the influenza epidemic. It is possible that this food shortage worsened the mortality from influenza during the 1918–1919 outbreak. However, it is not possible to gauge the likely scale of any effect of this kind.
· How many deaths were there in Sri Lanka during 1918–1919 as a result of the influenza outbreak? The number of additional deaths during these two years implied by the differences between the estimated age-specific death rates for 1918–1919 and the ‘normal’ rates is about 51,000. This is probably a reasonable estimate, though taking account of the fact that the age-specific rates for 1918–1919 may be slightly too high might reduce this figure by two or three thousand. However, it does depend on the arbitrary assumption that the excess mortality during 1918–1919 which was due to malaria rather than influenza is exactly offset by the excess mortality due to malaria included in the so-called ‘normal’ rates as a result of the fact that two of the nine years on which they are based, 1911 and 1912, were bad years for malaria.
· In round numbers, then, some 50,000 people probably died in Sri Lanka during 1918–1919 as a result of the influenza outbreak, about 1.1 per cent of the population. Expectation of life at birth fell from the usual level of 31.5 years to 26.7 years: these values are based upon the ‘normal’ and the estimated 1918–1919 mortality rates. This was heavier mortality than was experienced in England and Wales, where possibly one in 200 (0.5%) of the population died in the epidemic. However, it was very much lighter than the mortality in India where … almost 5.5 per cent of the population died.
Second Study
A 2014 study by Siddharth Chandra and Dilshani Sarathchandra of Michigan State University on “The influenza pandemic of 1918-1919 in Sri Lanka: Its Demographic Cost, Timing, and Propagation” revisited some of the data used by Langford and Story. This study is also important for bringing out certain new aspects. In their conclusions they stated as follows:
“The influenza pandemic in Sri Lanka demonstrated some of the features of the 1918–1919 global influenza pandemic observed in other countries…The numbers of deaths on the island and affected different regions in at least two distinct and severe waves. Results of our research suggest a need to revise current estimates of influenza mortality in Sri Lanka due to the pandemic. In contrast with the existing high estimate of 91 600 deaths or 1.1% of the population, our point estimates of loss of population are 307 000 and 313 000 or 6.7% of the population. This finding calls into question the assertion that influenza mortality in Sri Lanka was ‘very much lighter than the mortality in India where according to Mills almost 5.5 percent of the population died. Our results show that the demographic impacts of the influenza pandemic in Sri Lanka were similar to and as severe as those of neighboring India. In terms of geography, the findings build on the earlier work of Langford and Storey. They confirm that the pandemic most likely entered Sri Lanka through Colombo in the south and support their suggestion about a parallel entry point in Mannar in the northwest.
“The pandemic first peaked in these two coastal port areas and then radiated from the west to the east. These episodes of peak mortality lasted about eight weeks from early October to early December of 1918. A number of districts in the central part of the island were not part of this dynamic. These central districts experienced a wave of peak mortality that lasted about six weeks from early February to mid-March of 1919 and that differed from the earlier wave in terms of its duration in the different districts that were affected by it. These findings suggest the existence of three separate epidemiologic zones in colonial Sri Lanka for influenza and perhaps even other diseases that followed a person-to-person mode of transmission. These three zones more or less coincided with patterns of ethnic distribution and population density; the largest ethnic group, the Sinhalese, were found chiefly in the central, western and southern parts of the island; ‘Ceylon Tamils’, defined as people of Tamil ethnicity but Ceylonese ancestry, was found mainly in the northern parts of the island; and ‘Indian Tamils’, defined as people of Tamil ethnicity but Indian ancestry, resided in the south-central part of the island. In addition, the north-central districts, which did not experience peak mortality during the autumn of 1918, were also the districts with the lowest population density.
“This feature very likely contributed to a peak mortality pattern that was altogether different from that experienced by the more densely populated northern and southern regions of the island. The spread of the pandemic across the three regions in distinct waves suggests some isolation of the main ethnic groups from one another, and impediments to person-to-person contact across ethnic lines and barriers of low population density. As far as the interplay between the global influenza pandemic and its occurrence in Sri Lanka is concerned, it appears that the northern and southern zones were directly linked to the global epidemiologic system. The sparsely populated central zone separated the northern and southern zones from each other, appears to have been isolated from the global system, and experienced a dynamic all of its own. This finding further suggests that geographic contiguity alone was not a sufficient condition for the transmission of the mortality wave and that other factors such as person-to-person contact across regions, or the lack of it, may have played an important role in the spread of the disease. Given the scarcity of studies that examine the spread of the 1918 influenza pandemic at a relatively high level of geographic and temporal resolution, it is hoped that the methods used in this paper will encourage scholars to develop a more complete picture of the pandemic in different locations, thereby illuminating the factors that facilitated or hampered its spread. These insights can then be leveraged to inform strategies to contain similar events in the future using our existing knowledge about the importance of social distancing and other relevant spatial features of populations.”(references omitted).
Ministry of Health
In 2012 a National Influenza Pandemic Preparedness Plan (NIPP) for Sri Lanka was prepared by the Epidemiology Unit of the Ministry of Health. It noted that in the 20th century, there were three pandemics; in 1918 (H1N1), 1957 (H2N2), and 1968 (H3N2) and the 1918 pandemic resulted in 20‐50 million deaths and the other two 1‐4 million deaths each. The NIPP contained the following conclusions and next steps:
“After the experience with the H1N1 pandemic the next influenza pandemic is closer than ever before. But there is no way of knowing how close it is and it could happen tomorrow, next year or in 10 years. Because of this unpredictability and the grave consequences expected from such an event on all aspects of social and economic life, there is an imperative to move forward in putting preparations in place to mitigate the eventual impact. For the Ministry of Health, this imperative is the mitigation of morbidity and mortality. The NIPP is therefore also a process. Financial and technical constraints are the main constraints of implementing the programme on influenza. The programme cannot be fully financed by the Government of Sri Lanka. For instance, although stockpiles of adequate quantities of necessary antiviral drugs are available in the country, procurement of pandemic vaccine would not be an easy task. In addition necessary laboratory equipment and hospital materials are still not adequate. Therefore, gaps in resources must be identified in order to implement the plan and prepare the country. The best possible time to raise funds is when the country is still in this post‐pandemic phase following the H1N1 pandemic during which donor agencies are keen to assist.
Next steps
The pandemic preparedness plan must be implemented according to the phases as outlined although the timing and emergency of the pandemic virus is unpredictable.
A work plan and budget for each activity must be outlined with responsible persons, timeline, and indicators for evaluating progress.
The process should be described in terms of key responsible agencies, individuals, and provide benchmarks and timelines for measuring progress.
Technical sub‐committees must review the issues in their areas and forward recommendations to NIPP as early as possible. If external technical assistance is required, this may be identified and requested.
The Plan should be shared with all stakeholders within and outside the Ministry of Health for cohesiveness
Socialization, advocacy and training at all levels of administration on all aspects of the Plan and current status must be discussed with appropriate stake holders
Risk communication should be coordinated and public education should be initiated
Government resources that can be made available for influenza preparedness and the gaps that remain must be identified so that resource mobilization can be undertaken
Appropriate “tabletop” exercises to prepare must be undertaken with all related partners in order to build capacity and improve coordination and response. These scenario simulations will allow identification of gaps and weaknesses as well as means to improve elements of the plan. “
Not much is available in the public domain as to what extent the Plan has since been successfully implemented.
Unfinished Agenda
Though the importance of social distancing and other relevant spatial features of populations were highlighted in the second study, social distancing has now become a major impediment in the control of COVID-19. The Ministry of Health plan referred to above is far too generic in its scope and vision. Despite Sri Lanka’s long-time commitment to the implementation of human settlement declarations at Habitat I and thereafter, a large proportion of low-level urban income earners still live in congested areas with limited water and sanitary facilities. The Tamil estate workers also live in hardly habitable tiny buildings (‘lines in estates’, as popularly known). According to UNICEF, malnutrition is endemic in certain areas among women and young children, making them vulnerable to chest infections. The much-publicized Green Revolution in the ’60s and ’70s failed to retain the initial momentum and over the year’s fertilizer shortages have become ubiquitous. Haphazard deforestation, and adverse weather conditions, have caused an imbalance in the environment-human beings’ harmonious equilibrium. The economy is under severe stress and this has implications for peace, order and good governance. COVID-19 struck Sri Lanka at the worst possible time as the country was just regaining from last year’s Easter Sunday attacks. However, it redounds to the credit of the President that the health and military authorities were soon galvanized into action rather than appointing commissions and committees to decide on what to do, which was the typical response during the past several years to deal with any crisis. The President’s new thrust on domestic agriculture as a substitute for the import of rice and vegetables augurs well for the future as a well-nourished population can hopefully withstand better certain viruses than malnourished individuals. Social distancing, spitting on the road and public places and not covering with a tissue or a handkerchief whilst sneezing or coughing must be part and parcel of health education lessons in schools if parents fail to educate their children. Congested living conditions must be quickly addressed with better settlement planning. Fake drugs for malaria and other diseases have been reported from many countries and the drug authorities need to be cautious in importing drugs without proper quality verification (see the guest editorial by D. C. Jayasuriya, “Counterfeits: Grappling with Issues”, WHO Drug Information, Vol. 6 (1), 1992). The domestic legislation, Quarantine and Prevention of Diseases Ordinance of 1897, is an anachronistic piece of legislation. There are no legal safeguards against stigmatization, even though in the wake of HIV/AIDS pandemic many countries introduced legal measures. Preliminary evidence suggests that long-term smokers may be more vulnerable to COVID-19 and it will be interesting to see whether enough support will be garnered among the community of policy- and law-makers to tame the tobacco industry’s insidious influence. Even after more than 100 years since the tragic 1918-1919 influenza pandemic, Sri Lanka is yet to achieve significant development in many areas which tend to breed and spawn viruses which can be better controlled with commitment and self-discipline accompanied by modern public health measures and treatment.